Clots that form in a leg or arm vein can be deadly; prevention is key.
Blood clots are lifesavers when they seal a cut. They can be dangerous, even deadly, when they form inside an artery or vein. A blood clot inside a coronary artery can trigger a heart attack; one inside an artery feeding the brain can set off a stroke. Inside a leg vein, a blood clot can cause deep-vein thrombosis. Never heard of it? You're in good company. In a survey conducted by the American Public Health Association, barely one-quarter of adults were aware of the disease, and even fewer were familiar with its signs and symptoms. That's a sad state of affairs for a circulatory disorder the U.S. Surgeon General and others say is a critical health problem that causes enormous health consequences and numerous deaths each year. To draw attention to this overlooked condition, the Surgeon General has issued a "Call to Action" on it.
Deep-vein thrombosis (DVT) is a clot that forms in a vein that runs deep inside a leg or arm. Pulmonary embolism (PE) is its most serious — and often deadly — complication. One or both strike upwards of 600,000 Americans a year, killing at least 100,000. That's as many deaths as caused by breast, prostate, and colon cancer combined. And one-third of the survivors are left with long-term health problems.
You may have heard of these two linked conditions as the misnamed "economy class syndrome." Air travel accounts for a tiny minority of deep-vein thrombosis or pulmonary embolism. Injury, immobilization, and clotting disorders are the big culprits.
Key points
- Deep-vein thrombosis — a blood clot that forms in a leg or arm vein — can have devastating consequences, especially if part of the clot breaks away and travels to the lungs (called a pulmonary embolism).
- Knowing the warning signs and seeking treatment quickly can save your life and prevent long-term complications.
- Prevention is key. Move your legs often, especially when seated for long periods. Stay hydrated. And ask your doctor about medication or other treatments if you, or one of your limbs, will be immobilized for a while.
|
Troublesome clots
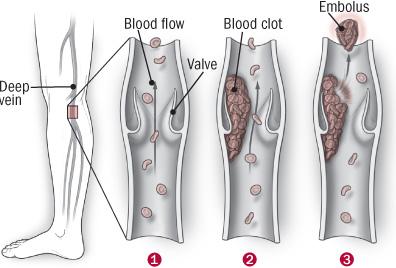
Blood that circulates to the legs and feet must flow against gravity on its journey back to the heart. The trip is aided by the contraction of leg muscles during walking or fidgeting. The contractions squeeze veins, pushing blood through them. Small flaps, or valves, inside the veins keep blood flowing in the direction of the heart.
Blood must keep moving to remain fluid. Anything that slows blood flow through the arms and legs can set the stage for a blood clot to form. This can range from having an arm or leg immobilized in a cast to prolonged sitting or being confined to bed. Things that make blood more likely to clot, such as genetic disorders and cancer, are other big triggers for deep-vein thrombosis.
When part of a clot breaks away and travels through the bloodstream, it is called an embolus. One that lodges in the lungs is called a pulmonary embolism. This is serious trouble. Pulmonary embolism kills about one in five people who have one.
Who's at risk?
Most people sail through life without ever experiencing a deep-vein thrombosis or pulmonary embolism. Others aren't so lucky. Factors that increase the chances of developing these conditions include the following:
- injury to a vein from a broken bone, severe trauma, or major surgery, especially surgery on the abdomen, pelvis, hip, or leg
- slow blood flow caused by prolonged bed rest, immobility due to a cast, or sitting for a long time
- taking hormones such as testosterone or estrogen (including birth control pills or postmenopausal hormone therapy)
- medical conditions such as factor V Leiden or other inherited clotting disorders, lung disease, inflammatory bowel disease, and cancer
- obesity, smoking, or a family history of deep-vein thrombosis.
|
Recognizing the signs
One of the big problems with detecting the presence of a deep-vein thrombosis or pulmonary embolism is that their signs and symptoms mimic those of a host of other conditions. Here are the most common warning signs:
Deep-vein thrombosis: pain or tenderness in a leg (especially in the calf, where it might feel like a charley horse that doesn't go away) or arm that gets worse with time, not better; swelling in one leg or arm; the skin of one leg or arm takes on a reddish or bluish color; one limb feels warm to the touch.
Pulmonary embolism: difficulty breathing; chest pain or discomfort that worsens with a deep breath or cough; coughing up blood; fast heart rate; sudden lightheadedness or fainting.
When coupled with a person's medical and personal history, one or more of these general signs should raise a red flag. Doctors usually search for a possible deep-vein thrombosis with ultrasound. Other tests include a venogram (a special x-ray of the leg) or MRI (magnetic resonance imaging). When pulmonary embolism is suspected, a blood test called the D-dimer test is usually done. It can detect an abnormally high level of blood-clot breakdown products in the bloodstream. A CT scan is also usually done.
Deep-vein trouble
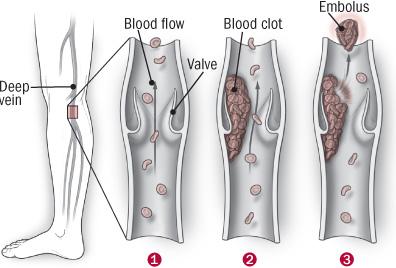
(1) Leg veins contain small valves that help keep blood moving toward the heart. Injury, immobility, and other factors can lead to the formation of a blood clot (2) inside a leg vein. This is called a deep-vein thrombosis. Sometimes a piece of the clot breaks away (3) (this is called an embolus) and enters the circulation. If it lodges in the lungs, it can cause a potentially deadly pulmonary embolism. |
Treatment
The main goal for treating deep-vein thrombosis is preventing pulmonary embolism. After that come easing symptoms and improving blood flow in the affected limb. Bed rest with the feet elevated, either at home or in the hospital, along with moist heat can help reduce pain and swelling.
Medications are also important. Heparin or other injectable blood thinners like low-molecular-weight heparin or fondaparinux (Arixtra) keeps the clot from getting larger and prevents new ones from forming. It is usually taken for five to seven days, and is then gradually replaced by warfarin (Coumadin, Jantoven, generic) for six months or longer. The use of compression stockings that squeeze the legs is also recommended.
The body's natural clot-busters gradually chip away at the clot. Sometimes it's important to speed the process along. This can be done by removing the clot with a procedure called venous thrombectomy or by injecting it with a clot-dissolving drug.
Treating pulmonary embolism is a far more urgent matter. Heparin and warfarin are used to stabilize the clot and to keep new ones from forming. Depending on the size and severity of the clot, additional treatments range from clot-dissolving drugs to physically removing the clot or placing a filter in the inferior vena cava, the large vein that carries blood from the lower half of the body to the heart.
The aftermath
For some people, a deep-vein thrombosis or pulmonary embolism is a one-time event caused by an injury or a temporary change in the blood's capacity for clotting. For others, it becomes a long-term health problem.
Having one deep-vein thrombosis or pulmonary embolism means you are at increased risk for another. About one-third of people who have a deep-vein thrombosis have another within 10 years. Men are three times more likely than women to have a recurrence.
When a blood clot damages one or more of the valves in a leg or arm vein, it can lead to chronic venous insufficiency, also called post-thrombotic syndrome. This can allow blood to pool in a leg, causing swelling or pain when standing. Damaged valves can cause varicose veins, discolor the skin, and even lead to painful skin ulcers.
Many survivors of a pulmonary embolism have long-term problems such as chronic shortness of breath, pulmonary hypertension, or heart failure.
Prevention, early detection are essential
You can take simple steps, literally, to prevent deep-vein thrombosis and pulmonary embolism. Moving your legs is the best medicine. If you have to sit for several hours at a time — on a plane, in a train or car, at work, or even at home — try to get up and move around as often as you can. While sitting, help your muscles push blood back to the heart by raising and lowering your heels while keeping your toes on the floor, raising and lowering your toes while keeping your heels on the floor, and tightening and releasing your leg muscles. Avoid wearing stockings that bind your calf muscle. And drink plenty of water.
If you've had a deep-vein thrombosis or pulmonary embolism, talk with your doctor about whether taking a blood-thinning medication like warfarin is right for you. Wearing compression stockings that gently massage the legs when traveling, or if you know you will be sitting for long periods, might also be a good idea. And try to keep up with the exercises listed above.
If you are confined to bed with an injury, after surgery, or during an illness, ask your doctor if you need medication or other strategies to prevent the formation of blood clots. Although most cases of deep-vein thrombosis or pulmonary embolism occur in hospitals or nursing homes, doctors often fail to identify and treat individuals at high risk for developing these potentially damaging conditions.



 پاسخ با نقل قول
پاسخ با نقل قول